Abstract and Introduction
Abstract
Neuroimaging has been pivotal in identifying and reframing our understanding of functional movement disorders. If accessible, it compensates for the limitations of the clinical exam and is especially useful where there is overlap of functional symptoms with classical presentations of disease. Imaging in functional movement disorders has increasingly identified structural and functional abnormalities that implicate hypoactivation of the cortical and subcortical motor pathways and increased modulation by the limbic system. Neurobiological theories suggest an impaired sense of agency, faulty top-down regulation of motor movement and abnormal emotional processing in these individuals. This framework challenges our traditional understanding of functional movement disorders as distinct from the deceptive term of 'organic' diseases and proposes that these conditions are not considered as mutually exclusive. This update summarizes the literature to date and explores the role of imaging in the diagnosis of functional movement disorders and in detecting its underlying molecular network.
Introduction
Functional movement disorders (FMDs) describe involuntary movements and posturing that are not in keeping with a known neurological cause.[1] They comprise 2–3% of all movement disorders, but there is a lack of population-based data so the true prevalence remains uncertain.[2,3] FMDs can mimic a range of known movement disorders, including tremor, dystonia, myoclonus, gait disorders and parkinsonism.[4] However, these movements are often distractible and entrainable unlike in classical manifestations of disease.[5] They can also accompany atypical behaviours like grimacing, sighing, extremely slow movements and whole-body movements with simple motor tasks.[5]
Functional disorders can either occur independently or accompany classical illness, which makes the distinction challenging with examination alone.[6,7] Functional neuroimaging is a means to address this limitation and can further clarify the nature of complex clinical presentations. Increasing research in this field has revealed that functional neurological disorders are associated with distinctive imaging changes, which has further informed several theories about its underlying pathophysiology.[8] In identifying the neurobiological models of FMDs, we begin to appreciate it as a new disease entity and identify potential avenues for treatment.
We performed a systematic review of the existing literature to identify how the role of imaging extends beyond the benefits of distinguishing FMDs from classical movement disorders. We also review the imaging advances in functional neurological disorders, particularly highlighting their insights into the functional and structural connectivity in this condition.
Terminology
Functional disorders have been previously referenced as psychogenic, somatization or conversion disorder. These terms imply that the symptoms are derived from a psychological trigger, which is not a requirement to diagnose functional disorders.[9] While terminology plays a key role in distinguishing from malingering or feigning symptoms, an accurate term has been challenging because of a limited understanding of the underlying physiology of functional disorders.[4] Invoking a psychogenic cause in the absence of identifiable risk factors falsely labels individuals. Based on a study by Stone and colleagues,[10] the term 'functional' was the most preferred by patients.
Search Strategy and Selection Criteria
The articles used for this review were identified using PubMed. Search terms included combinations of 'imaging', 'functional movement disorders', 'psychogenic movement disorders', 'MRI', 'SPECT', 'MEG' and 'PET'. All English language articles until 15 June 2020 were screened for relevance, and read in their entirety if they were suitable. The 17 articles that fit the criteria are summarized in Supplementary Table 1.
Diagnostic Clarification
Imaging can play a vital role in the diagnosis of functional movement disorders, especially when diagnostic clarity cannot be obtained with clinical exam alone. Dopamine transporter single-photon emission computer tomography (DAT-SPECT), detects presynaptic dopaminergic deficit, and can distinguish degenerative parkinsonism from mimics such as essential tremor, drug-induced parkinsonism, and functional parkinsonism with high sensitivity and specificity.[2,11,12] When DAT-SPECT (using TRODAT-1) was used on five individuals with clinically established functional parkinsonism, two demonstrated a presynaptic dopaminergic deficit, attributing their presentation to an underlying neurodegenerative aetiology instead.[11] Similarly, DAT-SPECT (using 123I-FP-CIT) revealed a neurodegenerative aetiology in two of three patients initially suspected to have functional parkinsonism.[13] In a study of nine individuals with suspected functional parkinsonism, further testing on the individual with bilateral decrease in 123I-FP-CIT striatal uptake further identified a parkin (PRKN) gene mutation.[14] Imaging can also establish the diagnosis of functional parkinsonism by demonstrating normal DAT density uptake.[15] In a study of 33 inconclusive cases, 123I-FP-CIT SPECT identified nigrostriatal degeneration in nine patients.[16]
Other useful imaging modalities include PET and MRI. PET using dual fluorodopa, which quantifies presynaptic nigrostriatal dopaminergic function, and fluorodeoxyglucose (FDG), which assesses metabolic function, was used to clarify the underlying aetiology in two patients with functional parkinsonism who presented for deep brain stimulation surgery. Both patients had normal caudate and putamen 18F-fluorodopa uptake on PET imaging and normal metabolism in the regions typically affected in neurodegenerative parkinsonian disorders.[17] In a 66-year-old male with gait instability, left laterocollis, intermittent mutism and verbal perseveration attributed to a FMD, had an FDG-PET which showed hypometabolism in the occipital lobe suggestive of dementia with Lewy bodies instead.[18] Elmalı and colleagues[19] describe a case of a 31-year-old female who presented with a postural and action tremor that was irregular and altered in direction, prompting the diagnosis of a functional tremor. However, MRI brain revealed abnormal thalamic and pontine signal changes suggestive of an alternative pathology. A family history of cirrhosis prompted the workup for Wilson's disease, with which she was subsequently diagnosed.[19] Similarly, a 20-year-old male with a variable, distractible rest and postural tremor in the arms had a spine MRI that revealed atrophy at the C5-7 level with anterior displacement of the dura with neck flexion. This was suggestive of Hirayama disease and with surgical intervention, his tremor improved up to 3-months follow-up.[20]
Perhaps where imaging is most useful is in the diagnosis of FMDs that coexist with classical pathology.[6,7] This is particularly challenging because FMDs can demonstrate a good placebo response to intervention, likely due to involvement of the mesocorticolimbic pathways.[3,6] When evaluating nine patients who were referred for suspected functional parkinsonism, 123I-FP-CIT SPECT confirmed diagnosis in three, and five patients had a combination of functional and degenerative parkinsonism. The remaining patient was attributed to the latter category based on clinical suspicion but had a normal SPECT scan. Long-term follow-up for an average of 2.3 years supported the diagnoses.[21] In another study by Lang and colleagues,[6] F-DOPA PET in four individuals revealed diminished unilateral striatal uptake in one individual, suggesting an overlap with degenerative parkinsonism. However, it is important to recognize that access to sophisticated neuroimaging techniques can be limited in low- and middle-income countries. This can risk misdiagnosis in challenging cases and result in poorer outcomes.
Insights Into Pathophysiology
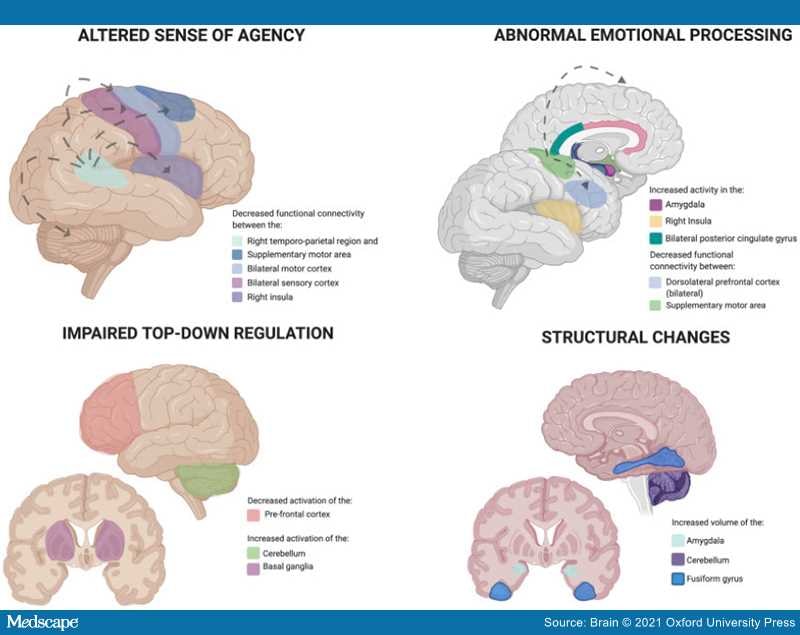
Functional imaging studies demonstrate that individuals with FMDs have altered patterns of cerebral activation, thereby suggesting genuine pathology instead of feigned deficit.[22–24] They demonstrate structural and functional differences from normal controls, particularly with the cortical and subcortical structures involved in the regulation of movement and emotion.[24,25] In addition to findings from other functional neurological disorders, there have been several neurobiological theories about the pathophysiology of functional disorders (Figure 1).
Figure 1.
Neurobiological models proposing the pathophysiology of functional neurological disease. Created using BioRender.com (by S.S.)
Altered Sense of Agency
This implies that individuals perceive their actions as involuntary, despite the distractibility and entertainability of movements on clinical exam.[26,27] It appears to be secondary to impaired sensorimotor feedback integration in FMDs, because of the reduced functional connectivity between the right temporo-parietal junction and bilateral sensorimotor areas, cerebellum, supplementary motor area (SMA) and right insula compared to healthy controls.[28] Individuals with functional paresis also demonstrate decreased activity in the supramarginal gyrus, which combines somatic and environmental cues that facilitate the initiation of movement.[29]
In a functional MRI study where individuals with FMDs performed a virtual reality movement task to modulate sense of agency, the dorsolateral prefrontal cortex (DLPFC) and pre-SMA on the right were unaffected by the loss of movement control. This suggests that in FMD, individuals remain unaware of a lack of activation.[30] When individuals with functional motor weakness were compared with healthy controls who were feigning weakness, passive movement of the weak hand increased activity in different regions, which also supports an altered sense of agency.[31]
Similarly, when functional tremor was compared to voluntarily mimicked tremor, individuals with functional tremor showed decreased activation of the right temporo-parietal junction and in the connectivity between the sensorimotor cortex and cerebellum.[32] As such, the sensorimotor feedback integration is impaired in functional disorders and the movement is not self-generated.
Czarnecki and colleagues[8] studied cerebral perfusion differences between functional tremor, essential tremor and healthy controls. At rest, individuals with functional tremor demonstrated increased relative cerebral blood flow (CBF) in the left inferior frontal gyrus and left insula. During motor task imaging, there was increased CBF in the cerebellum and reduced CBF in the anterior regions of the default mode network. The default mode network has been implicated in being active when the brain is at wakeful rest and an individual is not focused on a task. Its reduced activation in functional disorders suggests an impairment in self-representation and agency.[7,8]
Abnormal Emotional Processing
Functional weakness correlated with reduced activity in the SMA and increased activity in the right amygdala, insula and bilateral posterior cingulate cortices, which suggests preferential activation of the regions involved in emotional processing rather than movement initiation.[33] During internally generated movements, there was also reduced functional connectivity between the left SMA and bilateral DLPFC.[33] Unilateral functional leg weakness was associated with reduced regional CBF and increased activation of the orbitofrontal and anterior cingulate cortices.[34] These regions are implicated in emotional processing, especially in that of prior traumatic experiences.[34] When exposed to fearful and happy faces, individuals with functional weakness demonstrate a lesser difference in the activation of the right amygdala compared to healthy controls. This suggests a tendency towards increased excitability and decreased habituation.[33]
Individuals with a functional tremor exhibit increased activation of the right cerebellum compared to those with essential tremor, despite performing the same motor task.[35] In a basic emotion task, they also had increased activation in the paracingulate gyrus and left Heschl's gyrus compared to healthy controls, and decreased activation in the right precentral gyrus compared to individuals with essential tremor.[35] When the experiment was repeated in functional dystonia, in response to the basic emotion task, there was reduced activation of the right middle temporal gyrus and bilateral precuneus, and increased activation in the right inferior frontal gyrus, fusiform gyrus, bilateral occipital cortex and cerebellum.[36] With the intense-emotion task, they demonstrated decreased activation of the left motor and insular cortices, as well as activation of the left fusiform gyrus. However, in non-functional dystonia, there was reduced activation of the right opercular cortex and right motor cortex.
Impaired Top-down Regulation
Individuals with functional hand weakness demonstrated diminished functional MRI activation in the contralateral precentral gyrus, superior frontal gyrus, insula, occipital gyrus and ipsilateral cerebellum while observing movement, compared to healthy controls.[37] This reflects an impairment in the conceptualization of movement rather than active inhibition of the frontal lobe.[37] This observation was also replicated with PET imaging, where attempted movement of a functionally weak left hand was associated with decreased activation of the left DLPFC.[38] While attempting to move a feigned weak left hand, there was hypoactivation of the right anterior PFC, implicating impaired inhibition in the PFC in the pathology of functional weakness.[38]
Despite external stimulation in individuals with unilateral sensorimotor impairment, SPECT imaging revealed decreased regional blood flow in the contralateral thalamus and basal ganglia.[39] This hypoactivation had normalized with symptomatic improvement, suggesting that functional pathology may be attributed to impaired projections between the frontal cortex and basal ganglia.[39] In a task comparing functional left hand paralysis with healthy controls and feigners of paralysis, functional weakness was associated with activation of the ventromedial PFC during motor initiation.[25] In absence of movement, the precuneus and ventrolateral prefrontal gyrus were activated instead of the right frontal region, which is typically implicated in inhibition.[25] However, the right frontal region was activated during assessment of the unaffected hand. When the weakness was feigned, the frontal regions were activated in both the affected and unaffected hand.[25] This suggests that in functional disorders, there are different neuro-modulatory mechanisms that result in the absence of movement.
Using PET imaging of regional CBF, Schrag and colleagues[40] demonstrate that functional dystonia is associated with greater activation of the cerebellum and basal ganglia and decreased activation of the primary motor cortex. In contrast, in patients with genetic (DYT1) dystonia, there is increased activation of the motor cortex and thalamus and reduced activation of the cerebellum.[40] Abnormal activation of the right DLPFC during movement was the same in functional and non-functional dystonia. This suggests that while both represent abnormalities in motor attention, they do so by different mechanisms.[40] In a functional MRI study of nine individuals with FMD before and after rehabilitation, there was a significant shift in activation from the visual cortex, hippocampus and cerebellar vermis to the putamen, caudate and SMA. This reflects a shift in a bottom-up to top-down control of motor function.[7,41]
Structural Changes
Morphometric MRI has detected changes in regions associated with emotional processing, suggesting stress-mediated neuroplasticity in individuals with functional weakness.[7,42] Individuals with FMDs demonstrate an increased volume of the left amygdala, striatum, cerebellum, fusiform gyrus and bilateral thalamus but this does not correlate with duration or severity of the presenting illness.[43] It is unclear whether these represent premorbid characteristics that make these individuals susceptible to FMDs, or if they occur as a consequence of it.[43]
One study pointed out a correlation between mental health impairment, increased anxiety and increased right amygdala volumes.[44] The same group also described an inverse correlation between the degree of physical impairment in FMD and the volume of the left anterior insula on imaging.[44] They also demonstrated that individuals with higher depersonalization scores have an increased thickness of the right lateral occipital cortex compared to healthy controls.[45] Functional hemiparesis also correlated with increased thickness of the premotor cortex compared to healthy controls.[46] However, the consistency of these structural changes are inconsistent in the literature.
Individuals with functional dystonia have reduced volume of the right thalamus, bilateral caudate, precentral and frontoparietal cortices compared to healthy controls.[47] This suggests a reduced functional connectivity between the insula, right basal ganglia, dorsolateral prefrontal cortex and precuneus.[47] Another study by Nicholson and colleagues[48] revealed a significant reduction in the volume of the left thalamus in patients with FMD, regardless of severity of symptoms or laterality of deficit. Interestingly, children with functional motor and sensory symptoms also demonstrate these structural changes compared to healthy controls, suggesting that these findings can occur is the absence of primary psychiatric comorbidities.[49]
Limitations in Existing Research
The heterogeneity of the studies, small sample sizes and poor reproducibility challenge our ability to make meaningful conclusions about the imaging changes currently described in the literature. Functional disorders can be associated with altered emotional processing and psychosocial stressors,[50] which also limits the interpretation of the structural changes in the limbic system as we cannot link cause and effect.
The manifestation of the FMDs can also be varied, ranging from parkinsonism to myoclonus and tremor, and it is unclear whether the same neural circuits can be implicated for all presentations. Furthermore, distinctive features that differentiate the type of movement that is manifested (i.e. hyperkinetic movement disorders versus functional paralysis) have not been elucidated, and most the existing literature about the neurobiological circuitry are derived from studies about functional paralysis. Lastly, there are no longitudinal studies on this subject, so it remains unclear whether a subset of FMD patients with normal imaging eventually develop typical manifestations of disease.
Brain. 2021;144(8):2278-2283. © 2021 Oxford University Press