This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I'm Dr F. Perry Wilson of the Yale School of Medicine.
One of my first clinical rotations as a medical student was the pediatric emergency room. On my second day there, a 6-year-old was brought in with an ulnar fracture. He had fallen from a jungle gym. I stood aside, like a frightened medical student does, and watched as an incredibly talented ER nurse put an IV into the screaming child and administered… something.
In seconds, the kid was calm. The screaming stopped. Not asleep, his eyes were open, but he wasn't exactly… there. The orthopedic team quickly set the fracture and put on a cast. That was it. Within about 20 minutes, he was fine. Up and around, talking to his parents. Getting an ice cream.
That substance the nurse administered? Ketamine. I had never seen anything like it. To be honest, I still haven't. It is just a fundamentally different anesthetic.

Ketamine for the acute pain of a broken bone is relatively safe and highly effective. But what about chronic pain, like the pain of fibromyalgia or peripheral neuropathy? The data suggest that it may help — but the reason it may help could surprise you.
Chronic pain and depression feed into each other in a vicious circle of suffering.

Epidemiologically, the comorbidity of depression and chronic pain is incredibly high: 85% of those with chronic pain also have depression, and between 50% and 80% of those with depression have chronic pain. The causality can be hard to untangle and probably goes in both directions: Depression makes pain feel worse, and chronic pain leads to more depression.
The medical use of ketamine to treat resistant depression has exploded over the past 10 years, thanks in part to some studies suggesting nearly miraculous, long-lasting remissions within hours of a single dose.

As the data have filled out, the early reports of ketamine as a miracle antidepressant sobered up a bit. The Cochrane Collaboration's latest evidence synthesis suggests that ketamine can be useful for refractory depression, but the effect is short-lived.
Several studies have shown that ketamine may be effective for treating depression in those with chronic pain. But what about the reverse? Can ketamine be used — should ketamine be used — as a chronic painkiller?
Researchers from the National Institute of Health and Medical Research in France, led by Gisèle Pickering, tried to untangle the complex knot.
In a prospective study appearing in JAMA Network Open, they report on 329 patients receiving repeated ketamine infusions for the treatment of chronic pain across 30 French pain clinics.

This was a diverse group in terms of source of the chronic pain. Just over 50% had fibromyalgia, 30% with peripheral neuropathy, 6% with complex regional pain syndrome, as well as a smattering with other diagnoses. On a 10-point scale, at the start of the study the mean pain score was 6.8.

The dose of ketamine and the frequency of dosing were determined by each clinic, so the range is pretty wide. Over the 12 months of study, the mean cumulative dose was 444 mg. It seems like people were probably getting on the order of 0.5 mg/kg every month or so, but obviously that's variable.
This is a study about chronic pain, and chronic pain scores decreased rapidly — pretty much from the start of the study — by about 1 point on that 10-point scale.

That was statistically significant, but realize that we're going from about a 7 to about a 6. Not a miracle treatment, for sure, but then again, chronic pain is notoriously difficult to treat; some patients — and doctors — would take what they can get.
Depression scores improved as well, as expected, given prior studies. There were 123 individuals who met criteria for clinical depression at the start of the study and 94 by month 12. That's not nothing.

Where the study really piqued my interest was in its mediation analysis.
The authors wanted to know why chronic pain scores decreased. After all, the half-life of ketamine is about 2.5 hours. Even with frequent infusions, its direct anesthetic effect doesn't really explain pain control.
A mediation analysis looks for intermediate steps along the causal pathway to see what process mediates the observed effect of, in this case, ketamine on pain control.
And there was a big mediator. Honestly, I've done some mediation analyses, and this is really a massive mediator. Fully 64% of the observed effect was mediated by depression. In other words, the way that ketamine helps chronic pain is not through analgesia but through its antidepressant effect.
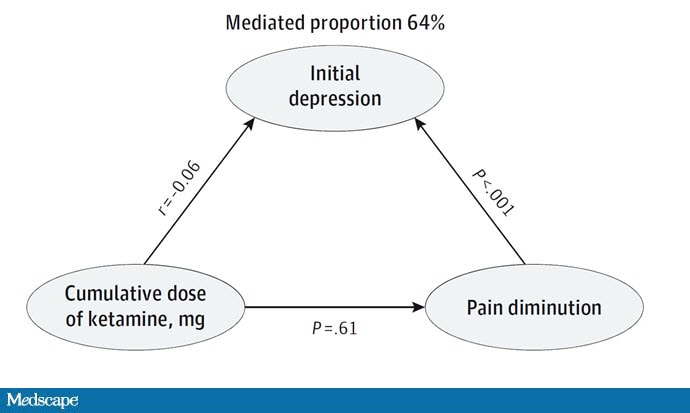
The authors also investigated whether the cumulative dose of ketamine helped with pain control. It didn't. All of the effect seems to run through the initial improvement in depression that occurs within that first dose. It's a compelling result, and for those who know their pharmacokinetics, not entirely unexpected.
To be sure, this study has limitations. The biggest one is that there was no control group — everyone in this study received ketamine, although the doses varied — so we might be seeing regression to the mean: people enrolling when their pain is relatively high, and who tend to come back to their baseline over time. But that doesn't explain the difference by depression scores, of course.
We're seeing an explosion in the use of ketamine for non-anesthesia-related reasons. To be honest, the data probably don't support the broad enthusiasm. But my gut tells me that the drug may be a reasonable antidepressant. This study shows us that it might work for chronic pain as well, but probably only as a side effect of its antidepressant property.
For Medscape, I'm Perry Wilson.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale's Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his new book, How Medicine Works and When It Doesn't, is available now.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
Credits:
Figure 1: Shutterstock 1852903981
Figure 2: F. Perry Wilson, MD, MSCE
Figure 3. Ketamine Prescriptions Increasing, Especially for Mental Health Treatment. Epic Research. May 5, 2023.
Figure 4. JAMA Network Open
Figure 5: F. Perry Wilson, MD, MSCE
Figure 6: JAMA Network Open
Figure 7: JAMA Network Open
Figure 8: JAMA Network Open
Medscape © 2023 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: F. Perry Wilson. Ketamine, Pain, and Depression: A Special Connection - Medscape - May 24, 2023.









Comments