Thirty-seven million adults in the United States and 537 million adults worldwide have diabetes.[1] By 2045, diabetes prevalence is projected to grow by 16% to affect 783 million people worldwide. While diabetes is associated with numerous medical complications, cardiovascular disease remains the leading cause of morbidity and mortality among persons with diabetes, often presenting earlier and in a more severe form than among individuals without diabetes. Diabetes confers a higher risk of multiple forms of cardiovascular disease, including ischemic heart disease, heart failure (HF), stroke, and peripheral artery disease, each of which has distinct implications for prevention and management strategies.[2] Therefore, understanding and addressing cardiovascular disease risk is a principal consideration for improving clinical outcomes in patients with diabetes.
In this issue of Circulation, Sattar et al[3] analyzed [almost equal to]680 000 patients with diabetes in the Swedish National Diabetes Register and [almost equal to]2.6 million age-, sex-, and county-matched controls to examine patterns in the incidence rates of multiple cardiovascular outcomes (ie, coronary artery disease, myocardial infarction, cerebrovascular disease, and HF) among persons with diabetes over the past 2 decades. Between 2001 and 2019, there was a continuous decline in rates of atherosclerotic cardiovascular disease (ASCVD) events among individuals with diabetes. The incidence rate (per 10 000 person-years) of acute myocardial infarction decreased from 74 to 41, coronary artery disease from 205 to 80, and cerebrovascular disease from 84 to 46. These ASCVD trends contrasted with the trends for HF among individuals with diabetes. After a period of declining HF rates from 1999 to 2013, the incidence of HF in diabetes plateaued over the past 5 years of follow-up. Furthermore, when modeling time period as the exposure, risks for acute myocardial infarction, coronary artery disease, and cerebrovascular disease have decreased over time among persons with diabetes and matched controls. In contrast, although the risk for HF has decreased slightly over time in controls, HF risk has increased temporally in those with diabetes. This work highlights a substantive shift in the predominant phenotype of cardiovascular disease in diabetes, with HF to become the most frequent cardiovascular complication in diabetes if current trends persist.
Observational studies demonstrate a powerful dose-response relationship between the degree of hyperglycemia in diabetes and the risk for adverse cardiovascular outcomes.[4] Therefore, maintaining glycemic control has long been considered a cornerstone of type 2 diabetes management. However, although intensive glycemic control reduces the risk for microvascular complications, it has a modest effect on macrovascular complications, has no significant effect on survival and confers markedly increased risk for hypoglycemic events.[5] More favorable results have been achieved by collectively addressing the multiple risk factors that are commonly associated with type 2 diabetes. The Steno-2 trial of 160 Danish patients with type 2 diabetes and albuminuria evaluated the cardiovascular effect of comprehensive risk factor control on clinical outcomes. Over 8 years, intensive intervention with behavior change and pharmacological therapy as needed to achieve control of glycemia, blood pressure (BP), and cholesterol, compared with conventional therapy, resulted in a 59% reduction in cardiovascular events, a 57% reduction in cardiovascular death, and a 46% reduction in all-cause death.[6]
The current study by Sattar et al[3] further highlights the importance of multifactorial risk factor control for cardiovascular outcomes in diabetes. Individuals who met target levels of hemoglobin A1c, systolic BP, low-density lipoprotein cholesterol, and estimated glomerular filtration rate and were nonsmokers had lower risks of ASCVD, with hazards that were comparable to or even lower than those of the control group without diabetes. The favorable ASCVD trends described by Sattar et al[3] track closely with the substantial improvement in control of several cardiometabolic risk factors observed among individuals with diabetes over the past 2 decades.[7] During that time frame, data from the United States demonstrate that the proportion of adults with diabetes achieving lipid control rose from 25% to 56%, and BP control rose from 39% to 48%, both correlating with the increased use of pharmacological therapies. Public health campaigns and policy changes have significantly reduced smoking rates. Sattar et al[3] found that in addition to hemoglobin A1c level and duration of diabetes, low-density lipoprotein cholesterol level, BP, and smoking had the greatest relative variable importance for coronary and cerebrovascular events among a comprehensive list of covariates. Therefore, this analysis provides compelling evidence that improved collective control of these traditional risk factors is succeeding in lowering the incidence of ASCVD among persons with diabetes.
In contrast, this analysis also demonstrated that individuals with diabetes who had all 5 major risk factors (hemoglobin A1c level, systolic BP, low-density lipoprotein cholesterol level, smoking, and estimated glomerular filtration rate) at target levels still had a 50% higher risk of HF than control patients without diabetes. The reason for this difference is the distinct pathophysiological pathways linking diabetes and associated comorbidities to ASCVD versus HF outcomes. Several risk factors had similar risk gradients for ASCVD and HF events, including hemoglobin A1c level, BP, and estimated glomerular filtration rate. However, cholesterol measures, BP, and smoking each had a substantially lower relative variable importance for HF compared with that seen for coronary and cerebrovascular events. Most notably, higher body mass index had a unique and steep risk association with HF that was not seen for other cardiovascular outcomes. Body mass index alone accounted for >30% of the excess risk of HF among individuals with diabetes. This finding corresponds with the known potent independent association between obesity and HF,[8] as well as the synergistic association of obesity and diabetes with HF incidence.[9] The complex interplay between diabetes and obesity includes the formation of advanced glycation end products, activation of inflammatory pathways, and increased oxidative stress, which lead to cardiac fibrosis, hypertrophy, and impaired myocardial function, commonly referred to as diabetic cardiomyopathy. Therefore, the observed plateau in HF incidence rates in recent years likely reflects the effect of the historically high rates of obesity in the population. In an important sensitivity analysis, when body mass index was added to the multifactorial risk factor control analysis, there was no longer excess risk for HF in those with diabetes. This highlights the critical importance of addressing obesity in addition to other traditional risk factors for fully addressing HF risk in diabetes.
The analysis had some important limitations that should be acknowledged. Cardiovascular risk factors were not measured in the control group, and these individuals likely had substantial heterogeneity in their cardiometabolic risk profiles. Furthermore, the investigators were unable to account for the development of diabetes in the control group after baseline. These unaddressed risk factors may have influenced rates of cardiovascular disease events in the control group, particularly among those with excess weight and greater insulin resistance at baseline, who were more likely to develop diabetes during follow-up. This analysis evaluated the trends of various cardiovascular outcomes in a Swedish cohort, in which the burden of obesity is much lower than in the United States (17%[10] versus 43%).[11] With a greater prevalence of individuals with both obesity and diabetes, the adverse trends in HF rates in diabetes may be even more striking in the United States.
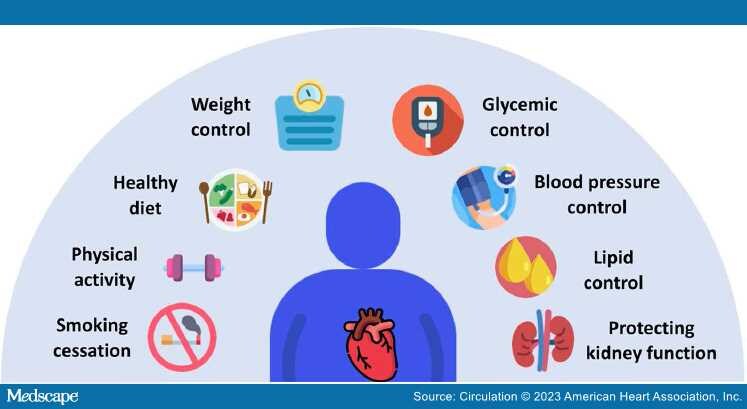
Major medical organizations emphasize the importance of a multifactorial approach to reduce the cardiovascular complications of diabetes, with a strategy including glycemic control, BP control, lipid control, and use of pharmacological agents for diabetes, with cardiovascular and kidney benefits[12,13] (Figure). As per interventional trials, an approach of lifestyle modification with additional targeted pharmacological therapy as needed to achieve risk factor control is optimal. However, a recent analysis indicates that only 22% of adults with diabetes have all 3 of the major cardiometabolic risk factors controlled.[7] A key barrier to achieving enhanced multifactorial risk factor control is adverse social determinants of health, which affect the development of diabetes, the likelihood of optimal self-care, and the risk for cardiovascular and other complications in diabetes. Therefore, addressing social determinants of health is key for optimizing management for individuals with diabetes. However, even after optimizing glycemic control, BP, cholesterol level, and smoking status, a substantial increased risk for HF will persist, largely as a consequence of the effects of excess adiposity. With overweight and obesity being present in 90% of adults with diabetes,[14] applying established strategies to improve weight management, including support for lifestyle modification, with adjunctive therapies of pharmacotherapy and bariatric surgery when needed, are critical to changing the current trajectory of HF in persons with diabetes.
Figure.
The importance of multifactorial risk reduction in the management of diabetes.
Optimal cardiovascular risk reduction in diabetes involves glycemic control in addition to blood pressure control, lipid control, and therapies to protect kidney function. Weight management, with intentional weight loss in those with overweight or obesity, is particularly critical for addressing heart failure risk in diabetes. Smoking cessation and lifestyle modification, including healthy diet and physical activity, are recommended for all patients, with additional pharmacological therapy as needed to achieve control of cardiometabolic risk factors.
The potential for cardiovascular risk reduction in diabetes has been further bolstered by the emergence of cardioprotective antihyperglycemic agents. The cardiovascular benefits of these agents include improved HF outcomes, enhanced renal protection and reductions in cardiovascular death for sodium-glucose cotransporter-2 inhibitors, and reduction of major adverse cardiac events and cardiovascular death for GLP-1 (glucagon-like peptide-1) receptor agonists.[13] GLP-1 receptor agonists also improve insulin resistance and induce substantial weight loss, particularly at higher-dose formulations. Because the indications for and effects of these agents cross organ systems and subspecialties, there is a need for more coordinated interdisciplinary care involving endocrinology, nephrology, cardiology, primary care, and additional complementary health care providers for the optimal management of diabetes-related risk, particularly when it is accompanied by other cardiometabolic comorbidities. Such interdisciplinary care approaches for diabetes have been shown to increase provider prescription rates of cardioprotective medications;[15] however, data demonstrating the downstream clinical benefits are not yet available.
We applaud the authors for their important work demonstrating the trends in cardiovascular outcomes in a large, population-based cohort of individuals with diabetes. Although improved glycemic, lipid, and BP control, as well as lower rates of smoking, have likely played a substantial role in progressive declines in rates of ASCVD, the historic obesity epidemic persists and has begun to shift trends for HF in diabetes, with HF poised to become the leading cardiovascular complication in diabetes. The analysis by Sattar et al[3] clearly demonstrates that in diabetes, a glycemic focus alone is not sufficient. There is a need to comprehensively control cardiometabolic risk factors, including overweight and obesity with both lifestyle and pharmacological therapies; to address social determinants of health that are closely linked to diabetes and its complications; and to develop and apply coordinated, interdisciplinary approaches to support optimal cardiovascular risk reduction for patients with diabetes and multiple comorbidities.
Circulation. 2023;147(25):1887-1890. © 2023 American Heart Association, Inc.