Abstract and Introduction
Abstract
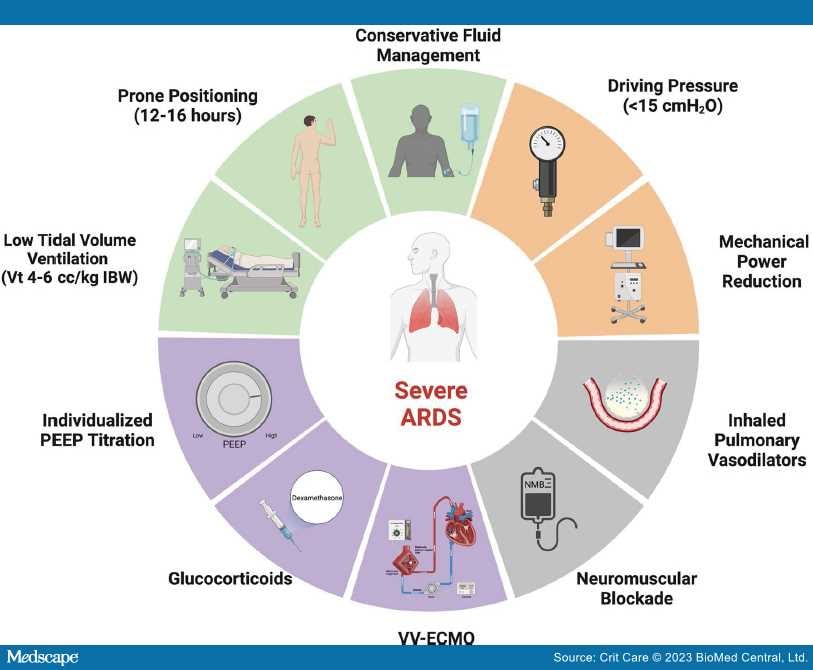
This narrative review explores the physiology and evidence-based management of patients with severe acute respiratory distress syndrome (ARDS) and refractory hypoxemia, with a focus on mechanical ventilation, adjunctive therapies, and veno-venous extracorporeal membrane oxygenation (V-V ECMO). Severe ARDS cases increased dramatically worldwide during the Covid-19 pandemic and carry a high mortality. The mainstay of treatment to improve survival and ventilator-free days is proning, conservative fluid management, and lung protective ventilation. Ventilator settings should be individualized when possible to improve patient-ventilator synchrony and reduce ventilator-induced lung injury (VILI). Positive end-expiratory pressure can be individualized by titrating to best respiratory system compliance, or by using advanced methods, such as electrical impedance tomography or esophageal manometry. Adjustments to mitigate high driving pressure and mechanical power, two possible drivers of VILI, may be further beneficial. In patients with refractory hypoxemia, salvage modes of ventilation such as high frequency oscillatory ventilation and airway pressure release ventilation are additional options that may be appropriate in select patients. Adjunctive therapies also may be applied judiciously, such as recruitment maneuvers, inhaled pulmonary vasodilators, neuromuscular blockers, or glucocorticoids, and may improve oxygenation, but do not clearly reduce mortality. In select, refractory cases, the addition of V-V ECMO improves gas exchange and modestly improves survival by allowing for lung rest. In addition to VILI, patients with severe ARDS are at risk for complications including acute cor pulmonale, physical debility, and neurocognitive deficits. Even among the most severe cases, ARDS is a heterogeneous disease, and future studies are needed to identify ARDS subgroups to individualize therapies and advance care.
Introduction
The acute respiratory distress syndrome (ARDS), first described in 1967,[1] is a common cause of respiratory failure in the ICU. There are approximately 190,000 ARDS cases annually in the USA alone, although cases skyrocketed in 2020 due to the COVID-19 pandemic.[2,3] ARDS pathophysiology is rooted in the disruption of the alveolar capillary barrier by inflammatory and oxidative insults. This results in the characteristic clinical (acute onset), radiographic (bilateral alveolar opacities), physiologic (reduced compliance, high shunt fraction), and histologic (classically diffuse alveolar damage) derangements. Severe ARDS, defined by an arterial partial pressure of oxygen (PaO2) to fraction of inspired oxygen (FiO2) ratio (P/F) ≤ 100, carries mortality close to 50%.[2] In moderate-to-severe ARDS, positive end expiratory pressure (PEEP) may confound the P/F ratio, and is addressed using the "P/FP ratio" ((PaO2*10)/(FiO2*PEEP)), with P/FP ≤ 100 defining severe ARDS.[4] The noninvasive ratio of pulse oximetric saturation (SpO2) to FiO2, or the "S/F ratio", also correlates well to P/F ratios and is readily available at the bedside. Though not clearly defined, S/F ratios of < 89 to < 120 approximate severe ARDS.[5–7]
Patients with severe ARDS are at high risk for ventilator-induced lung injury (VILI) and may develop refractory hypoxemia and hypercapnia. Traditional treatment of severe ARDS is supportive, anchored by lung protective mechanical ventilation, proning, and conservative fluid management.[8–10] Adjunctive therapies (e.g., inhaled pulmonary vasodilators, glucocorticoids) can be used, and in select cases, patients may require veno-venous extracorporeal membrane oxygenation (V-V ECMO). This review will summarize the evidence-based management (Figure 1) of severe ARDS emphasizing interventions that improve outcomes.
Figure 1.
Severe ARDS Treatments. A schematic illustrating management strategies for severe ARDS and refractory hypoxemia. Green sections represent treatments that improve outcomes supported by prospective randomized controlled trials, the orange section represents a treatment that may improve outcomes based on retrospective data, the gray sections represent treatments that may improve oxygenation but have not demonstrated sustained clinical benefit in trials, and the purple sections represent treatments that likely derive benefit in a subset of patients. ARDS acute respiratory distress syndrome, IBW ideal body weight, V t, tidal volume; and V-V ECMO, veno-venous extracorporeal membrane oxygenation. Adapted from "Risk Factors of Dementia," by BioRender.com (2023). Retrieved from https://app.biorender.com/biorender-templates
Crit Care. 2023;27(289) © 2023 BioMed Central, Ltd.
Copyright to this article is held by the author(s), licensee BioMed Central Ltd. This is an Open Access article: verbatim copying and redistribution of this article are permitted in all media for any purpose, provided this notice is preserved along with the article's original citation.