This transcript has been edited for clarity.
Carolyn A. Chan, MD: Welcome back to The Curbsiders addiction medicine podcast, where we use expert interviews to bring you clinical pearls and practice-changing knowledge on substance use disorders. I'm Dr Carolyn Chan, and I'm joined by my good friend, Dr Natalie Stahl. Can you tell the audience what we're going to be doing today?
Natalie Stahl, MD, MPH: We're going to recap recent episode number 18 on urine drug testing with our guest, Dr Timothy Wiegand from the University of Rochester.
Chan: He gave us so many great pearls, so be sure to check out the full podcast episode, Urine Drug Testing. Dr Wiegand reminded us that before we even order a urine drug test (UDT), we should be sure to let the patient know what the purpose of the test is and how it will be used to guide clinical care. Don't order a UDT if you don't have a purpose for it. When you have the results back, be sure to be supportive, not accusatory, and ask questions, particularly if there are unanticipated results.
Persons with substance use disorders have already experienced stigma in the healthcare system, so be sure to avoid stigmatizing language such as dirty and clean, and instead try to use terms like positive and negative when referring to UDT results. UDT results should be used to help support a patient in recovery, and the patient should be involved in the dialogue surrounding their test results.
For example, say you're following up with a patient in your buprenorphine program and their UDT suggests that they may be having some challenges taking the medication. You might say something like, "Your urine test was negative for buprenorphine and positive for fentanyl. Was this expected for you?" Then let them engage in the dialogue and go from there.
What different types of UDTs are available?
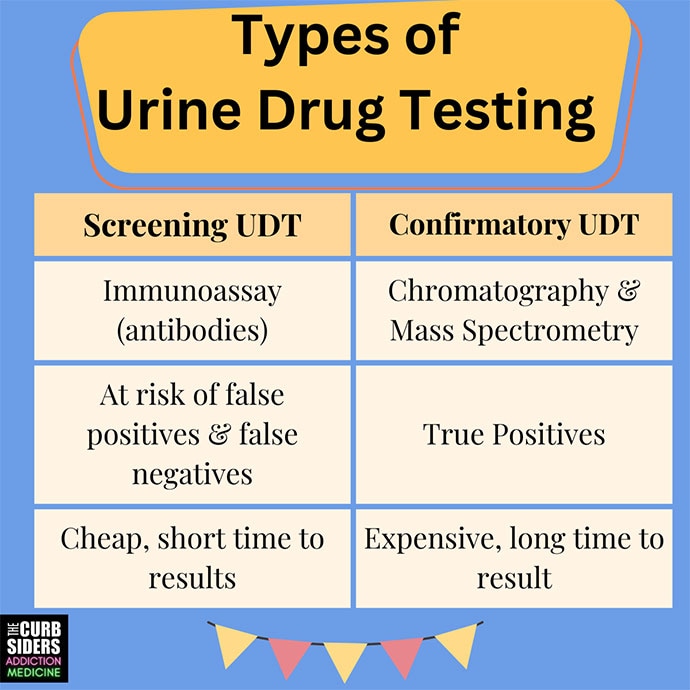
Stahl: Generally, there are two types of UDTs: screening Immunoassays (which use antibody technology) and confirmatory testing (uses gas or liquid chromatography paired with mass spectrometry).
The screening immunoassays test for common panel substances — a standard panel for a given institution — and results can be obtained quickly. The screening tests are cheap, so this is what we will encounter most often in the clinical setting, but we have to be cautious in interpreting them. They are screening tests; they are not perfect. Other substances can cross-react with antibodies, producing false positives. False negatives can occur also.
Since these test results can have a big influence on management or other consequences down the road, we must be mindful of potential false positives and the implications. Common medications that can cause false positives for amphetamine in a screening UDT, for example, include bupropion, pseudoephedrine, and over-the-counter Vicks decongestant (which contains l–methamphetamine). So, technically, it's a true positive, but it's not the illicit amphetamines that we might be looking for.
A common medication that can cause a false positive for benzodiazepine is sertraline, which is often used to treat anxiety. Medications that can cause positive phencyclidine results include dextromethorphan, carbamazepine, tricyclic antidepressants, and venlafaxine.
If you want to avoid a false positive, confirmatory testing is often accessible, but it's more expensive and it takes longer to get results back. Will it impact patient care or change your management? Is this a high-stakes legal scenario, such as a patient involved with child protective services or on probation? In situations where it might affect their lives to have a false positive, think about doing confirmatory testing.
What were some of the pearls on interpreting opiate and opioid UDT results?
Chan: With the opioid overdose crisis, physicians prescribing opioids for pain or treating opioid use disorder often use UDTs to monitor adherence or progress. But it's important to interpret these results carefully because it's not always straightforward. And in my practice, I honestly find this to be one of the more challenging tests to interpret.
Opiates are different from opioids. Opiates are substances derived from an opium plant (such as codeine or morphine), whereas opioids are synthetic or semi-synthetic (such as oxycodone, fentanyl, or hydromorphone). False positives are common on these immunoassays. False-positive results for opiates can occur with opioids such as hydromorphone, and naloxone and naltrexone can cause false-positive results for oxycodone. Drugs that can cause false-positive fentanyl results include risperidone, trazodone, and even labetalol. If we do see a positive on a screening immunoassay, it may make sense to order a confirmatory test to determine which substances the patient was taking. You'll want to have an opiate and opioid metabolism chart in front of you when you interpret these tests.
Why might a UDT result come back as invalid?
Stahl: Validity testing is a way to ensure that the urine sample is a good specimen. The lab report can provide markers that give insight into the validity of the specimen. One of these is temperature, which should be around body temperature shortly after voiding. The urine creatinine level tells us whether the sample is too dilute or too concentrated. If it's outside the normal range, it's not valid. There could be physiologic reasons that a sample is too dilute, or the patient might have added water to the sample or drank a lot of water prior to doing the test. The pH and specific gravity of the urine should be within the normal range. You may have to order these validity markers separately.
Although we want to avoid the possibility of invalid samples, we also want to minimize the intrusion involved in obtaining a urine sample. For example, minimize observed urine drug testing because many patients have a history of trauma and it can really influence their relationship with treatment providers. The American Society of Addiction Medicine (ASAM) recommends considering alternatives to an observed urine drug test, such as saliva testing. It's a great option.
This is a lot of information and it’s complicated. We often need our charts in front of us to double-check everything. It’s hard to remember all these details, but ASAM provides a good resource, Appropriate Use of Drug Testing in Clinical Addiction Medicine Consensus Document.
Follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Credit: The Curbsiders
© 2023 WebMD, LLC
Cite this: How to Interpret a Urine Drug Test - Medscape - Sep 06, 2023.











Comments