This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to The Curbsiders. I'm Dr Matthew Watto, here with my great friend, Dr Paul Nelson Williams. Paul, how's it going tonight?
Paul N. Williams, MD: It's going great.
Watto: We are reviewing our podcast called Hypercoagulable Work-Up With Dr Jean Connors. Let's start. What might make you think that someone has a family history or predisposition toward clotting?
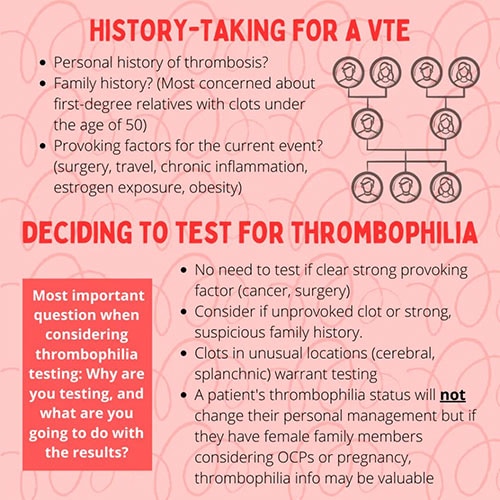
Williams: Something I had not previously fully appreciated was how important age is, but it sort of makes sense. Age is kind of protective against everything. If a younger patient goes through something that is potentially coagulopathic and develops a clot, that's a bit of a trigger, and the same goes for family members.
First-degree relatives under age 50 who have seemingly unprovoked clots should at least raise your eyebrows a little bit. It doesn't necessarily mean you have to test, but it does suggest that there might be some sort of heritable thrombophilic state that you need to think. And then there are other fascinating risk factors, such as obesity.
Watto: I'd heard that obesity was a risk factor, but Dr Connors quantified it. She said obesity (a BMI of 30-40) is as big of a risk factor as being heterozygous for factor V Leiden, which increases your risk for clotting to about three times that of the average population, as does taking an oral contraceptive pill. And these risk factors are all stacked together. If someone has obesity and heterozygous factor V and they are taking an oral contraceptive pill, then their risk is really high. You have to think about these things when you're talking to patients who have had a clot — or family members with a clot — and ask about these risk factors. She said that some surgeries are pretty strongly provoking, specifically the orthopedic, intra-abdominal, and neurologic surgeries. But if someone has a clot after a superficial surgery, that can be suspicious of a lower threshold due to the presence of some kind of inherited thrombus failure.
Williams: Just to tie the bow on the clear provoking factors, I think cancer is number one. That's the nuisance type of provoking factor, and you don't have to go down a rabbit hole of fancy-pants hematologic workup.
Watto: Patients always want to be tested when they have a clot. People just want to know. And clinicians seem to love to order these tests. However, I always try to do this with every test I order. I ask myself, what am I going to do with the results of this? Why am I ordering this testing? Our guest made this point about provoked and truly unprovoked clots. The patient with a provoked clot is going to be treated for the course of that provoked clot. The patient with an unprovoked clot has a good case for indefinite anticoagulation. So it's probably not going to change much for the patient.
But Paul, why might it be worth testing?
Williams: It goes back to that heritable factor. For example, if your patient's daughter is thinking about starting oral contraceptives or is considering pregnancy, you want to know if that patient might have passed that on to their progeny, increasing their risk. It might be helpful in terms of counseling patients about family members who may benefit from further testing to quantify their risk.
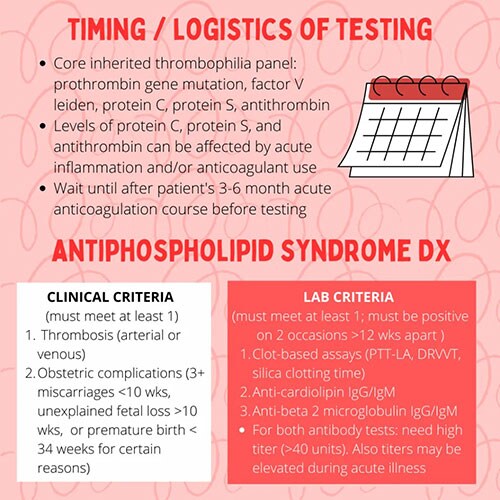
Watto: Of the five most common tests you might order, the prothrombin gene mutation and factor V Leiden can be sent any time because they are genes; the antithrombin, protein C, and protein S are very sensitive to what's going on in the body. You don't want to test those while the patient is on anticoagulation or when the patient has active cancer or active inflammation; you're just not going to be able to interpret those results. Wait until they've completed their course of treatment. If they are on a DOAC like an oral anticoagulant, make sure they haven't taken it for a few days to a week before you test them. For patients on warfarin, you want to wait longer than 2 weeks before testing. Again, make sure you know what you're going to do with the test results.
One thing I thought was really shocking was what Dr Connors said about how she handles patients with a prior provoked clot who are going on a long (≥ 6 hours) plane trip.
Williams: Apparently it's not in the guidelines, although it sounded like Dr. Connors thinks it should be, at least as expert opinion. For patients who aren't being treated with lifelong anticoagulation but have declared themselves to be somewhat thrombophilic, and are going to be doing something that could be provoking, like a prolonged flight, she will prescribe prophylactic anticoagulation or a prophylactic dual oral anticoagulant just for the trip and counsel them around that. She may even give someone who travels a lot a supply of 30 pills so they can take them before long plane trips to reduce the risk of developing a clot while flying. It's a concept that makes perfect sense, but it had never occurred to me.
Watto: Great expert opinion that you won't hear anywhere else. I recommend that everyone listen to this podcast, because we go way into the pathophysiology and the details of how she makes her decisions. It's too much to cover on a short video, but you can check it out on this link.
Follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Image credits: The Curbsiders
© 2023 WebMD, LLC
Cite this: Matthew F. Watto, Paul N. Williams. When Your Patient Has Had a Clot: Expert Advice - Medscape - Aug 16, 2023.












Comments