Inflating a drug-coated balloon in the prostate is the latest approach to treating a common cause of frequent or difficult urination in older men.
As the prostate naturally grows with age, the gland can obstruct the flow of urine ― leading to frequent trips to the bathroom and disrupted nights. An estimated 50% of men aged 60 years and older have benign prostatic hyperplasia (BPH). That figure rises to over 80% by age 70 and to 90% by age 80.
Transurethral resection of the prostate was the main surgical treatment for symptomatic BPH for much of the 20th century.
More recently, researchers have developed various minimally invasive surgical therapy (MIST) devices to treat the obstruction while limiting effects on sexual function. Some newer devices use lasers or water vapor to remove prostate tissue. Another approach uses implants to move and hold prostate tissue out of the way.
Now drug-coated balloons have entered the picture.
With the Optilume BPH catheter system, urologists inflate a balloon to split the lobes of the prostate. A second balloon can further separate the lobes and deliver a drug, paclitaxel ― best known as a chemotherapy medication ― to limit further growth and keep the lobes apart.
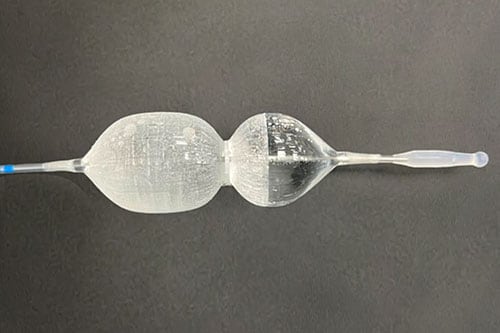
The Optilume BPH catheter system.
The US Food and Drug Administration approved Optilume BPH in June. The results from a randomized controlled trial of the device were published in the September issue of The Journal of Urology.
Uptake of MIST devices for BPH "has been variable due to a host of factors including mixed results, complexity of equipment, and costs," the journal's editor, D. Robert Siemens, MD, noted in the issue.
The developer of the device, Urotronic, said it expects that the newest treatment will be commercially available in the near future. Discussions about cost, insurance coverage, and how to train urologists to use it are ongoing, said Ian Schorn, the company's vice president of clinical affairs.
Raevti Bole, MD, a urologic surgeon at Cleveland Clinic's Glickman Urological and Kidney Institute, said BPH treatments ideally benefit patients for years, so she is eager to see how patients are doing 5 and 10 years after the Optilume BPH procedure. Studies should also examine its effects on fertility.
But given the safety and efficacy results reported 1 year after treatment, "I think this is something that a lot of people are going to be able to use in their practice and that their patients are going to benefit from," Bole told Medscape Medical News.
She said she expects most urologists will be able to master the technology. The procedure's minimal effect on sexual issues and the relatively short time needed to perform it are other advantages.
"All of those things are very positive in terms of whether patients are going to want to consider it and also whether surgeons are going to be able to realistically learn it and offer it at their centers," Bole said.
In choosing a particular treatment, Bole discusses options with patients and takes into account factors such as trial data, the nature and severity of symptoms, treatment goals, comorbidities, and the size of the prostate.
Available MIST devices can vary by institution, and urologists can have different levels of experience with each device. If a patient is interested in an approach a surgeon does not offer, the surgeon can refer the patient to a colleague who does.
Active vs Sham Treatment
Urologists may be familiar with another Optilume device, the Optilume urethral drug-coated balloon, that is used for urethral strictures.
The devices have similar names, and the underlying technology is similar, but there are major differences, Schorn said.
The BPH device expands between the lobes of the prostate, creating an anterior commissurotomy. A double-lobe balloon locks the device in place during inflation.
For the PINNACLE trial of the BPH device, which was conducted at 18 sites in the United States and Canada, Steven A. Kaplan, MD, of the Icahn School of Medicine at Mount Sinai, in New York City, and colleagues enrolled 148 men with symptomatic BPH who were experiencing urinary flow obstruction.
The average age of the patients was 65 years; 100 of them were assigned to undergo active treatment with Optilume BPH. The rest received a sham procedure that mimicked active treatment.
At 3 months, men who received active treatment had an average improvement in the International Prostate Symptom Score of about 11 points. This improvement was maintained at 1 year. Those who received sham treatment experienced an 8-point improvement at 3 months that dissipated over time.
The rate of urine flow increased dramatically with Optilume BPH, the researchers reported.
Five serious adverse events were considered to be possibly related to the device. There were four cases of postprocedural hematuria that required cystoscopic management or extended observation, and one case of urethral false passage that required extended catheterization.
Nonserious adverse events in the men who underwent the Optilume procedure typically resolved in about a month and included hematuria (40%), urinary tract infection (14%), dysuria (9.2%), urge or mixed incontinence (8.2%), mild stress incontinence (7.1%), bladder spasms (6.1%), elevated prostate-specific antigen levels (6.1%), and urinary urgency (6.1%), according to the researchers.
In a subset of participants for whom pharmacokinetic data were available, systemic exposure to paclitaxel was minimal.
Four participants in the Optilume BPH arm (4.1%) reported ejaculatory dysfunction, compared with one man in the sham treatment arm (2.1%). There were no cases of treatment-related erectile dysfunction.
Most patients were treated under deep sedation or general anesthesia, and the average procedure time was 26 minutes.
After the procedure, patients received a Foley catheter, which remained in place for about 2 days, "which is not significantly different from water vapor thermal therapy, holmium laser enucleation of the prostate, or laser photovaporization in similar gland sizes," Bole and Petar Bajic, MD, also with Cleveland Clinic, noted in a commentary accompanying the article in The Journal of Urology.
MIST devices can be ideal for patients who prioritize sexual function, but the need for a temporary catheter after the procedure can be a "major postoperative source of patient dissatisfaction," they acknowledged.
"Consistent with other minimally invasive technologies, the Optilume BPH procedure is a straightforward procedure that can be conducted in an ambulatory or office outpatient setting with pain management at physician and patient discretion," Kaplan and his co-authors wrote.
The study was featured on the cover of the journal, which the research team saw as an unusual but welcome spotlight for a treatment for BPH.
"We were thrilled that we got on the cover of The Journal of Urology, which is not a common thing for BPH technology," Schorn said.
Urotronic funded the PINNACLE study. Bole has disclosed no relevant financial relationships.
J Urol. Published online September 1, 2023. Full text
For more news, follow Medscape on Facebook, X, Instagram, and YouTube.
Credits:
Images: Urotronic
Medscape Medical News © 2023 WebMD, LLC
Send news tips to news@medscape.net.
Cite this: Can This Device Take on Enlarged Prostates? - Medscape - Sep 07, 2023.






Comments